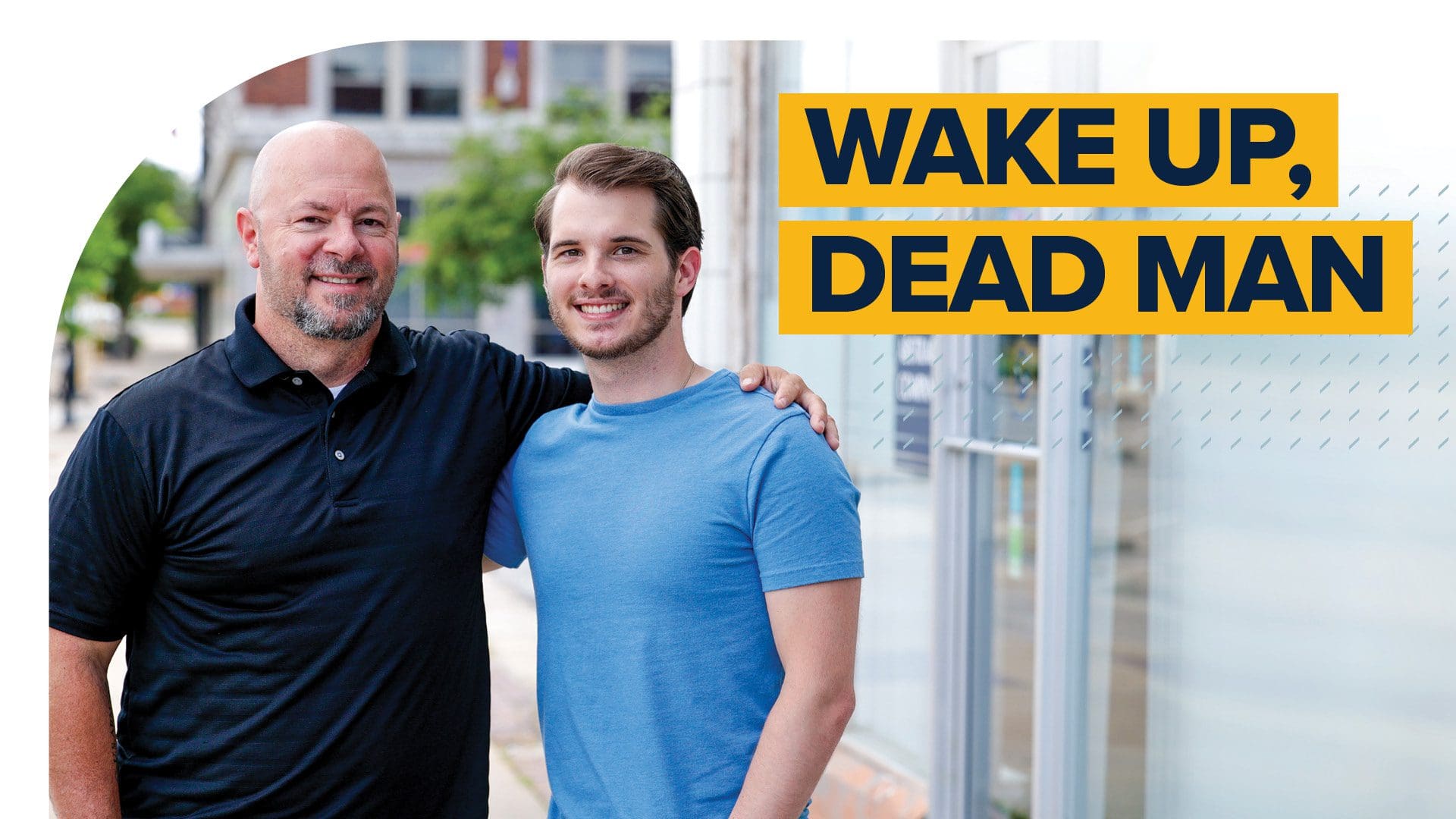
Wake Up Dead Man
In January of 2021, David Sieminskie was close to death.
Infected with COVID-19, he lay in the Intensive Care Unit of Hillcrest Medical Center, deeply sedated and struggling to breathe. His prognosis was grim, and Micah Neuenschwander, one of his nurses, knew it right away.
“The night that I first had him, he was already prone on his belly. He was sedated, he was paralyzed, he was on blood pressure support,” Micah recalls. “Most people I saw at that point didn’t make it out without permanent brain damage, to where they wouldn’t be able to function anyways. Or they just didn’t make it.”
On Micah’s second night with David, he worked to change the situation. The goal was simple: David had to wake up and start breathing on his own, getting off the ventilator and restoring his own functions. Through multiple nights, Micah tried to help him break through—with no success.
It took time, patience, and hope in the face of what seemed like insurmountable odds. “The night that he woke up, I honestly wasn’t expecting it,” Micah says. “I had gone the whole night, multiple times, trying to get him to wake up and open his eyes and do something for me. And I hadn’t had any success.”
But just as Micah’s shift was ending, something happened: David Sieminskie opened his eyes.
On Friday evening, symptoms began to appear. “It hit,” David says. “And it hit hard.”
“It was a complete game-changer,” Micah says. “As soon as he did that, I had to tell him: you have to keep fighting.”
He sat by David’s bedside, that phrase his rallying cry: keep fighting. Not just for David himself, but for his family, the people outside the hospital who needed him to recover. After that, Micah simply repeated his patient’s name, over and over, like a mantra:
David, David, David, David.
Realistically, David Sieminskie’s story should have ended differently. Both he and Micah know that. But it didn’t. And when asked to describe exactly what happened, to explain that pivotal moment, David’s answer sounds deceptively simple:
“I woke up to Micah screaming my name in my face,” he says, his tone matter of fact. Other than a few hazy blurs, it’s the first thing he can remember now of his two weeks in critical care.
The important thing is that he woke up at all. It wasn’t a given. Both David and Micah use the word miracle to describe it.
Uncommon Circumstances
In a kinder world—a world where healthy fifty-year-old men don’t end up half-dead in the ICU—David and Micah might never have met. Their paths certainly wouldn’t have converged naturally.
When the pandemic began in 2020, Sieminskie was a healthy salesperson in Collinsville, working to sell the PPE that would be so valuable later in the year. Micah was working to finish his senior year at OKWU amid the chaos that accompanied the Spring 2020 semester: delays, virtual classes, and a widespread, undefined sense of unease. He was already working as a nurse extern when the general COVID outlook began to look scary, but he tried to take a measured response to it.
“I think everybody had the same thought at first: it’s just another one of those diseases that’s going to come by, it’s going to leave, and that will be that,” he says. “It wasn’t until I got to the ICU that I really started to see how bad things got.”
Once that reality dawned, the emotional and physical toll was costly. “It’s not common for new grads to see as much death as what we have—all these new grads that are going into the COVID units now after graduating.”
David’s reaction to the pandemic was measured, too—at least in the beginning.
“My initial thought process was like anyone else’s: okay, how does this affect me?” he says. “Months went on, you learn more about this, and you understand just how real it is.”
His initial diagnosis was pneumonia on a Monday evening in January. On Wednesday, after an antibiotic, he was feeling better. It was later in the week that he thought to receive a COVID test. It was positive. On Friday evening, symptoms began to appear.
“It hit,” David says. “And it hit hard.”
That night, his wife Belinda took him to the local emergency room. It’s the last substantive memory he has until the moment he woke up to Micah’s voice.
“A Good Human Being”
Even after David woke up, Micah kept checking in, amazed at the progress his patient was making. “Even before he left the ICU, he was getting out of bed on his own, which is unheard of,” he says. “We couldn’t believe that he had been doing so well.”
When things progressed to the point that they could finally move David out of the COVID-specific ICU area and into a general section of the hospital, Micah checked in one last time. This time, he brought something with him.
“He came up there, and he’s checking on me and wondering how things were going. He brought me a card and said, ‘Thank you for allowing me to take care of you,’” David recalls now. “I mean… who does that? That’s just incredible.”
Micah says he’s given notes to a few patients during the COVID crisis. It’s a way to thank those people that he’s been able to help towards positive outcomes—because, as sad as it is, those positive outcomes were rare last year.
“David was one of my three success stories,” he says. “I wanted him to know that he has definitely changed my life… Patients like him and these other success stories that we have, that’s the reason why we go into nursing. And if I can have the chance to tell him that he’s the reason why I keep coming to work every night, then I definitely want him—and all my patients—to know that.”
When a local news station picked up the story, it provided an opportunity for the two to connect outside of the hospital. They friended each other on social media, began texting back and forth, and made plans to see each other, even as David struggled through a grueling physical therapy process.
It’s been months since that singular moment in a lonely hospital room in Tulsa, when a dying man awoke to life again. It’s fair to say both David and Micah remember it differently. For Micah, it’s an example of light during a dark year, a flicker of hope during a long, cloudy night.
For David, of course, it’s different. He’s simply grateful to be alive, pointing to the daunting recovery statistics for those who become intubated with COVID. “In terms of people making it, I absolutely consider it a miracle,” he says. “I’m one of the fortunate ones… I give God the glory and I always will.”
But he also views this story as a testament to the sacrifices those in the medical industry made last year, a way to shine a light on their stories. In his eyes, that’s the value of this story. It’s not about him at all; it’s about those men and women standing in the gap for their patients each day, an expression of Christian love—and OKWU’s mission—if ever there was one.
“Understand that these people are out there taking risks that most people don’t want to take,” he says, his voice passionate. “They deserve every bit of the accolades or recognition [they get]. And the beauty of it? Micah wasn’t interested in accolades or a pat on the back. He was more interested in how I was doing, in making sure I came out of it alive. That’s not just helping or being a nurse, that’s being a good human being.”